Background
The real-world experiences of Hemophilia A (HA) patients receiving emicizumab prophylaxis in China are insufficient due to the high cost and later approval of emicizumab. In this study, we retrospectively analyzed Chinese HA patients with or without factor VIII (FVIII) inhibitors receiving emicizumab prophylaxis with the aim to investigate the efficacy and safety of emicizumab as well as the current status and effect of different doses of emicizumab in a real-world setting.
Methods
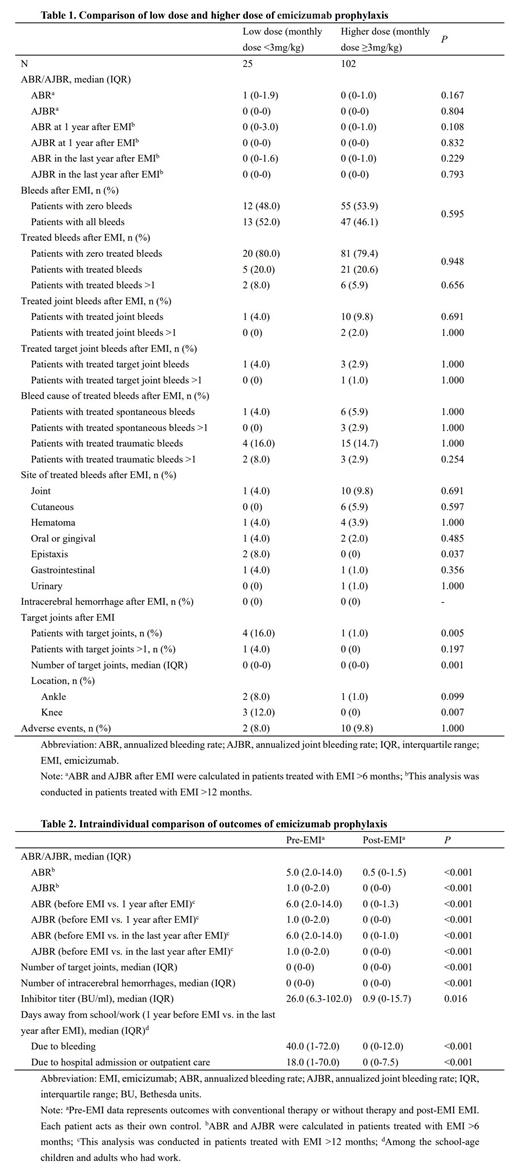
HA patients with or without FVIII inhibitors receiving emicizumab prophylaxis between June 2019 and June 2023 in China were included in the study. Data of HA patients including children and adults were retrospectively gathered from 27 hospitals all over the country. For each patient, the anonymized data were collected and telephone follow-ups were conducted to make sure the intact information collected as much as possible. Low dose and higher dose of emicizumab were defined as monthly dose <3 mg/kg and monthly dose ≥3 mg/kg, respectively. All analyses were performed using SPSS software version 25.0 (IBM Corporation, Armonk, New York, USA). Intraindividual comparisons were performed by nonparametric paired tests.
Results
A total of 127 male patients (10.2% [n=13] ≥18 years old; 89.8% [n=114] <18 years old) were enrolled in our study (severe: moderate = 103:24). Of these, 42 (33.1%) had FVIII inhibitors at initiating emicizumab. The median (interquartile range [IQR]) duration of emicizumab treatment was 16.0 (9.0-30.0) months.
The median (IQR) annualized bleeding rate (ABR) and annualized joint bleeding rate (AJBR) after emicizumab were 0.5 (0-1.5) and 0 (0-0), respectively (calculated in patients treated with emicizumab >6 months). Among the 127 patients, 67 (52.8%) patients had no bleeds at all. No intracranial hemorrhage occurred after emicizumab. Adverse events were reported in 12 (9.4%) patients and 10 (83.3%) were injection-site reactions. There were no deaths, thromboembolic events, or thrombotic microangiopathies in our study.
Two (8.0%) patients had treated epistaxis after emicizumab with low dose compared with 0 (0.0%) with higher dose ( P =0.037). Four (16.0%) patients had target joints after emicizumab with low dose compared with 1 (1.0%) with higher dose ( P =0.005) (Table 1). There were no significant differences between low dose and higher dose of emicizumab prophylaxis in ABR, AJBR, the proportion of zero bleeds, the proportion of adverse events, and so on.
The median (IQR) ABR was 5.0 (2.0-14.0) with prior treatment compared with 0.5 (0-1.5) with emicizumab, an 90% reduction in ABR with P value <0.001 (Table 2).Also, the use of emicizumab was also associated with significant reduction in AJBR ( P <0.001), number of target joints ( P <0.001), number of intracerebral hemorrhages ( P <0.001), inhibitor titer ( P =0.016), and days away from school/work ( P <0.001).
Conclusion
In this multi-center study, we indicated the efficacy and safety of emicizumab and that low dose and higher dose of emicizumab had similar efficacy in Chinese HA patients without increasing adverse events.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal